Coronary angioplasty and stenting is a method of treating coronary artery disease by restoring blood flow in the narrowed vessel that supplies blood to the heart. A heart catheterization is used to determine whether the procedure is indicated in each particular case.
What is cardiac stenting
The procedure is performed simultaneously with angioplasty. The latter allows to restore the coronary arteries lumen by introducing a balloon and inflating it. To prevent artery re-stenosis, a stent (a tubular metal mesh) is placed. It will keep the heart artery from narrowing again, ensuring normal blood flow.
Why is stenting performed?
Stenting is one of the most effective methods of coronary heart disease treatment. The intervention is used in patients with critical narrowing of the coronary vessel lumen. The procedure has the following advantages:
• it is easy;
• there is no loss of blood;
• general anesthesia is not required;
• the recuperation period is short;
• the risks of complications are minimal.
Indications for stent placement
The main indications are:
The main indications are:
• acute myocardial infarction;
• angina pectoris Grade 3-4 despite the adequate drug therapy;
• unstable angina;
• silent ischemia.
Possible contraindications to the operation:
• allergic reaction to iodine;
• blood clotting disorders;
• an artery diameter less than 2 mm;
• severe renal disease.
Alternative Methods
If there are reasons against using stents, a coronary artery bypass graft (CABG) is recommended. This method is preferable for complex multivessel coronary artery disease cases, since it reduces the possibility that a reoperation will be needed. Bypass surgery is also a better choice for patients with diabetes.
Some experts consider rotablation as an alternative treatment. In clinical practice, this technique is used in patients with severely calcified coronary lesions. The procedure involves “drilling through” the hardened plaque in a coronary artery. Its tiny crumbs are washed away by the bloodstream.
The treatment strategy is determined by a joint decision of a cardiologist and a heart surgeon. In case of doubt, a second opinion is recommended.
Coronary stenting in case of myocardial infarction
During the intervention, a stent is placed inside a vessel. This is a short, wire mesh tube that acts like a scaffold to help keep the artery open.
The stent is inserted into the affected artery following balloon dilatation performed with the help of a catheter. The purpose of the procedure is to prevent re-narrowing of the vessel. Nowadays, this technique is the most common and effective in the treatment of coronary heart disease.
What is a stent?
A vascular implant (stent) is a metal structure that resembles a tube-shaped mesh barrier. It can also be described as a tiny stretchable metal spiral with a diameter of 2 to 5 millimeters and a length of a few centimeters. The task the implant performs is to first widen the lumen narrowed by fatty deposits and then support it from the inside so that the artery does not close again. This ensures the free flow of blood through the vessel and minimizes the risk of occlusion caused by plaque.
Types of stents
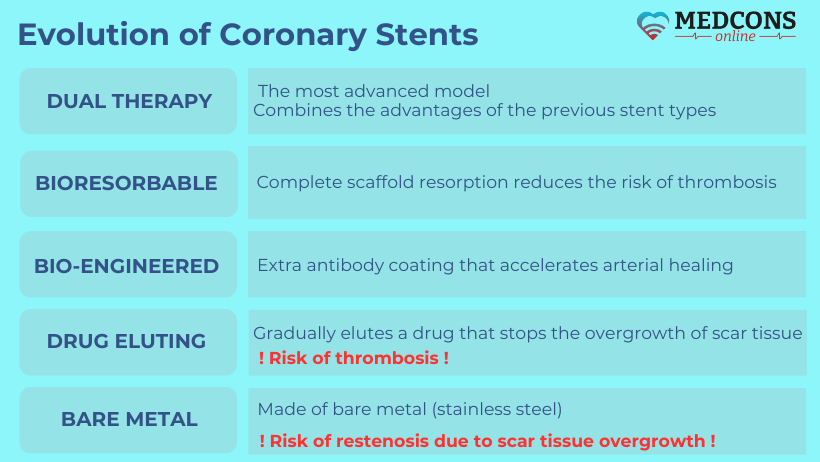
Depending on the patient's condition and indications, various stents can be used:
• uncoated metal stents;
• drug-eluting stents;
• biodegradable stents.
Initially, the procedure involved using bare-metal stents. Currently, drug-eluting scaffolds are used instead. They contain Paclitaxel, an anti-cancer medicine. Immunosuppressants like Sirolimus, Everolimus, Zotarolimus, etc. are also applicable. The substances make it possible to stop the process of tissue growth in the stent area for a certain period. This prevents the artery from getting narrow again.
According to statistics, the likelihood of re-stenosis with drug-eluting stents is less than 10%. In comparison, the probability of re-narrowing with bare-metal stents is 15-20%. Therefore, coated stents are particularly recommended for patients at high risk of restenosis. In addition, Sirolimus coating is superior in performance to other types of stents. The possibility of reoperation with these stents is minimal.
Drug-eluting stents are recommended for use in patients with thin arteries, extended stenoses, and diabetes mellitus.
Biodegradable stents are made from lactic acid polymers. Due to this, they completely dissolve after three years. Therefore, no foreign objects will remain in the body. Some of such stents may also be coated with a drug to prevent re-narrowing.
The correct choice of stent type is of key importance. Therefore, when in doubt, one should seek a second opinion from a reliable European expert.
How long does a stent last?
In principle, the lifespan of a vascular stent is unlimited, regardless of whether it was inserted after a heart attack or in the absence of a heart attack. It may happen that after some time the stent gets overgrown by tissue, so a new occlusion forms, but this does not mean that the implant must necessarily be replaced. If necessary, another one can simply be inserted. Removal of a stent once it was inserted is usually not necessary.
What is the difference between a stent and a shunt?
A stent is a kind of support structure that reopens the lumen of a blocked vessel or keeps it open for unimpeded blood flow. A shunt, on the other hand, is a diversion channel through which blood bypasses the blocked portion of the vessel. Catheter-assisted stent implantation is less complicated and less risky than a bypass operation, i.e., heart surgery. This is why it is generally considered as the first option when blood flow needs to be restored.
How do modern stents differ from older implants?
About 20 years ago, a stent was essentially a rather crude metal frame, as its ties were still relatively thick. They were over 100 micrometers in size, meaning they were larger than the diameter of a human hair. Nowadays, they are almost twice as thin. But the main difference is that when using the first-generation stents, the so-called restenosis, i.e. re-narrowing of the arteries, occurred more often. Modern implants consist of thinner elements and have a drug coating, which prevents restenosis.
How is stenting of the heart arteries performed?
The treatment starts with a coronary angiography. The procedure consists in obtaining photo and video images of the coronary vessels after injecting a contrasting substance. The technique is safe and highly informative. The findings determine the status of the atherosclerotic plaque and indications for stenting. They also help to choose the stent type, as well as its size and diameter.
In addition, a fractional flow reserve measurement and a cardiac MRI may be performed.
Step-by step description of the intervention:
• The doctor creates a puncture in a large artery (femoral, radial, brachial, ulnar) under local anesthesia. An incision is made on the skin, the wall of the artery is pierced, and a conductor is inserted. At the same point, the introducer is installed.
• A catheter is placed in the artery mouth, then a conductor is inserted below the narrowing of the vessel.
• A balloon is delivered along the conductor to the site of artery stenosis, with the help of which the affected area is pre-expanded.
• Next, under x-ray control, a balloon with a stent is inserted and installed at the site of the narrowing.
• The balloon is slowly inflated to reach the desired volume under a pressure of 10-14 atmospheres. Then it is deflated and removed.
• To check the stent placement, another coronary angiography is performed.
• Only then the introducer is removed, and the puncture site is covered with a sterile pressure bandage.
After the procedure is completed, the patient must remain in bed for 24 hours. The puncture site is carefully monitored for 24 hours. The bandage can be removed in a day.
Prognosis after treatment
Angioplasty and stent implantation significantly improve blood flow through the damaged artery. The severity and frequency of pain in the chest decrease, and the patients feel stronger.
It is important to understand that the procedure does not cure coronary disease. It allows one to get rid of the circulatory disorders which the condition causes. Thus, to achieve the best result, it is important to change your lifestyle, take the prescribed medications, and visit a doctor regularly.
If the disease-specific pain returns, and persists at rest, with no response to nitroglycerin, one needs to call a doctor immediately.
On the whole, life quality improves in 95% of patients. The positive effect lasts for at least five years.
Postoperative follow-up and management
With selective procedures, patients stay in the hospital no more than 2-3 days. After the intervention, a control examination is carried out, and the patient can go home upon receiving recommendations and prescriptions. One can return to a normal way of life in a week. After this period, it is allowed to return to work. If the procedure was performed due to a heart attack, the rehabilitation period can last up to a month.
To avoid complications, it is important to strictly follow the instructions of the doctor.
The main recommendations are:
• stop smoking and drinking alcohol;
• bring your body weight to normal;
• get your blood cholesterol level lower;
• stabilize your blood pressure;
• maintain an active lifestyle;
• control the blood sugar level.
Possible Complications
The complication rates are constantly decreasing. This can be attributed to technical improvements and novel drug support regimens. Physician expertise is also a major factor.
Possible complications include:
• spasm and dissection of the coronary artery;
• acute arterial occlusion;
• artery wall perforation;
• allergic reactions to drugs;
• infection at the insertion site of the catheter;
• ischemia of the lower extremities;
• nephropathy;
• bleeding from the puncture site;
• microembolism.
A thorough preliminary examination can prevent most of the complications.
The following symptoms may indicate a complication and make it necessary to see a docto:
• pain at the site of catheter insertion, hematoma, bleeding;
• discharge of pus from the puncture site, fever;
• sensation of cold in the hand, at the puncture site;
• excessive weakness, pain in the heart.
Restenosis of the coronary arteries
Restenosis is the recurrence of coronary artery narrowing after stenting. The reason is an excessive growth of the inner layer on the artery walls, which makes it difficult for blood to flow. It is considered a complication. Restenosis signs may occur 4-6 months after treatment. If it does not happen within a year after stenting, it is less likely to occur later.
Rehabilitation and medication
The chances of stenosis recurrence are lower if you follow your doctor's instructions. Blood thinners and cholesterol lowering drugs are a must. Antithrombotic medicines reduce the risk of blood clots forming on the metal stent walls.
As part of rehabilitation, it is important to avoid atherosclerosis risk factors. These are smoking, fatty foods, and a sedentary lifestyle. After stent placements, patients must see a cardiologist according to the recommended schedule.
What is allowed after stenting
The duration of rehabilitation is longer if the patient had a heart attack. Only after the acute period is over, is it allowed to get out of bed and perform simple physical exercises. During the first days, simple gymnastics is allowed in the prone position.
Walking is allowed after transfer to a regular ward. The duration of walks should be increased gradually. The volume of physical activity is controlled by a doctor.
To speed up recovery, it is recommended to stop smoking and alcohol, reduce fatty and salty foods, as well as the amount of salt (the latter should not exceed 4 grams per day).
Second opinion
The correct therapy choice is crucial in coronary artery disease. If you feel unsure, it is better to seek a second opinion. A consultation with European experts will help you understand whether the current treatment strategy is appropriate.
A second opinion may be useful at:
• Choosing the stent type. The experience of leading German specialists will guide you in selecting the best option with consideration to your health condition.
• Planning the drug therapy after treatment. It plays a great role, so it should be done very carefully.
• Considering alternative treatments. Stenting is not always the best way to handle a heart issue. In some cases, CABG may bring better results.
Angioplasty with stent implantation is an effective method of restoring normal blood circulation, including emergency cases of myocardial infarction. The procedure is not complicated, and is very effective in bringing patients back to a normal life, free of pain and other coronary artery disease symptoms.
References:
- Coronary artery stenting, Dale T Ashby, 2002.
- Coronary artery double stenting techniques and their results in complex left main bifurcation disease, Gianluca Rigatelli, 2020.
- Treatment of coronary artery in-stent restenosis, Damianos G Kokkinidis, 2017.
- Coronary artery stents: advances in technology, Sameer D Sheth, 2014.


Comments — 2
Галина
Спасибо. Очень доступно и грамотно. Я по диплому врач
ADAMOPOULOS DIMITRIOS
Hi! Is it possible to find out with a second opinion how much stenting was necessary? I had three stents installed last year. It was an emergency intervention caused by a heart attack. Could one or two stents be enough?