
Prostate cancer (carcinoma) is one of the most common malignant tumors in men. It occurs predominantly in people over 40 years of age, with the majority of cases being detected at the age of 50-70. Early diagnosis is made difficult by the fact that the disease is practically asymptomatic.
Disease definition
This type of malignancy develops from the epithelial cells of the organ. It progresses slowly enough, so there is a chance to detect and treat the disease in time.
Carcinoma can affect one lobe of the prostate or spread over the entire gland, sprouting into the urethra, bladder and other nearby organs. Cancer cells detached from the parent tumor first settle in nearby lymph nodes, and then, as the lesion grows, enter the bloodstream and get transported to distant parts of the body, giving rise to metastases in the liver, lungs and bones.
Prevalence
About 1.3 million new cases are registered annually in the world, including 449.8 thousand in Europe, 234.3 thousand in North America, and 297.2 thousand in Asia. The disease is observed practically on all continents of the planet. Among cancerous diseases in men, cancer is second only to lung cancer.
It is believed that after 80 years of age this pathology is found in the overwhelming part of the male population, but in many men it is in latent state (from the Latin “latentis” - hidden, invisible), so it has no clinically significant manifestations.
Causes
Although not all risk factors are yet known, the major ones include:
- Geography and ethnicity. African Americans who are residents of the United States have a 60% higher incidence of prostate carcinoma than white Americans. And Chinese people residing in their ancestral home have the lowest incidence rates.
- Genetic predisposition. The risk increases twice if a father or brother suffered from the disease, and 5-11 times if 2 or more relatives had it.
- Age. Among residents of the United States, for example, for every 100,000 people in the U.S. prostate cancer occurs in 44 people under the age of 65 years, and in 900 men 65-74 years.
Symptoms of prostate cancer
In the beginning, patients are usually unaware of the presence of a malignant tumor, and this may be the case for many years. Another option is that the manifestations of a malignant tumor are so similar to those of benign adenoma or ordinary inflammation (prostatitis) that even doctors can be misled without special laboratory and imaging tests.
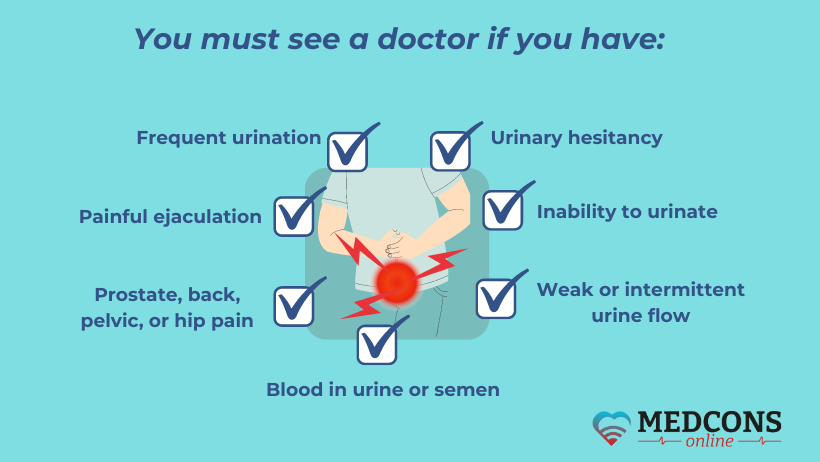
Symptoms of carcinoma are divided into several main groups associated with the following factors:
- Urinary disorders - intermittency of the urine stream or its weakening; increased frequency of urination (normal frequency for an adult is 4-9 times during the day and 0-1 times at night), a feeling of incomplete emptying of the bladder, involuntary urination during physical activity, laughter, coughing (stress incontinence), periodic uncontrolled urine leakage combined with a strong sudden urge to urinate (imperative urges).
- Local progression of the lesion - the appearance of blood in semen or urine (haematuria, haemospermia), varying degrees of erectile dysfunction, pain in the pubic area, perineum.
- The appearance of distant metastases - swelling of the lower extremities in case of violation of lymphatic outflow; pain in the bones, lumbar region; impaired sensitivity, paralysis of the lower extremities, etc as consequences of spinal cord compression.
How to recognize the first signs of prostate carcinoma
Since most neoplasms grow slowly enough, they do not show any signs for a long time. However, it is possible to suspect the pathology at the very beginning with the help of laboratory and imaging diagnostics, i.e. determination of PSA (prostate-specific antigen) level in the blood and transrectal ultrasound (TRUS). Therefore, experts recommend regular preventive examinations for all men aged 50 and older, or from an earlier age in the case of hereditary predisposition.
As the tumor grows, the increasing in size organ begins to squeeze the urethra. Because of this, many patients come to the doctor for the first time with complaints of impaired urination, such as:
- changes in the urine stream,
- difficulty urinating,
- stress incontinence or urges.
Less often, the disease first makes itself noticed by haematuria, haemospermia or erectile dysfunction.
Classification of prostate cancer. Treatment strategy depending on the disease spread
First of all, the TNM classification is used, which was last revised in 2017. It is based on 3 leading characteristics of any cancer process:
- T (tumor) - size and extent of the parent (primary) prostate tumor.
- N (nodulus) - lymph node involvement.
- M (metastasis) - presence or absence of distant metastases.
On its basis, oncologists usually distinguish 4 stages of the disease, taking into account both the local spread of the tumor and the presence or absence of distant metastases. For this purpose, such neoplasm imaging methods as ultrasound, MRI, CT, PET-CT, etc. are most often used.
Gleason and International Society of Urological Pathology (ISUP) scales are classification principles specific for prostate cancer. They are based on the results of biopsy and subsequent histological examination. The value of the Gleason index (IG) indicates the aggressiveness of the neoplasm, helps to better determine the choice of specific therapeutic procedures, and also gives an idea of the prognosis of the disease.
Learn more about the Gleason scale and the ISUP scale
By its nature, prostate cancer is a whole group of malignant tumors originating from epithelial cells. Depending on morphological features, they may be:
- adenocarcinomas – acinar, cribriform, papillary, solid/trabecular, endometrioid, glandular-cystic and mucinous;
- cancers - transitional cell and squamous cell.
As a rule, any malignant tumor is heterogeneous in its cell composition, and its type is determined by their predominant type. All of them differ in the speed and aggressiveness of growth, as well as the response to various therapies.
American pathologist Gleason in 1966 proposed to take into account the degree of of prostate cancer cell differentiation. Of these, highly differentiated tumors were considered to be the most non-aggressive and slow-growing, and those with low differentiation were considered aggressive. He divided them into 5 categories, assigning each type a certain score: 1 for the highest degree of differentiation, 5 for the lowest. But the main advantage of this scoring was that the final characteristic of the tumor took into consideration not only the cells that were mostly observed under the microscope (primary score), but the cells immediately following them in terms of their number or aggressiveness (secondary score). From these two numbers, a total Gleason score is obtained, which is used to determine prostate cancer treatment strategy.
Who calculates the scores. This is done by morphologists who study a fragment of a prostate tumor under a microscope.
ISUP. In 2014, a new classification based on the Gleason scale was developed by the International Society of Urological Pathology. In 2016, it was approved by the WHO, as it was more successful in avoiding unnecessary radical operations in case of clinically significant prostate cancer (slow growth, low aggressiveness of the neoplasm). ISUP has 5 prognostic groups. It is now used in conjunction with the Gleason index and represents its improved version.
How to interpret the results. 6 points is the minimum and 10 is the maximum score on this scale. The higher the figure, the more aggressive the tumor and worse the prognosis:
| Gleason score | ISUP or Gleason prognostic group (G) | Five-year recurrence-free survival of prostate cancer | Interpretation and treatment strategy |
| 6 (3+3) | 1 | 97,5% |
It is more often observed at the beginning of the disease. The tumor is characterized by rather slow growth and does not extend beyond the capsule of the prostate for a long time. Nerve-sparing surgery is possible. |
| 7 (3 + 4) | 2 | 93% | Moderately differentiated adenocarcinoma. The prognosis is quite favourable. Nerve-sparing surgery is indicated. |
| 7 (4 + 3) | 3 | 78,1% | Adenocarcinoma of medium malignancy. The tumor is dominated by aggressive low-differentiated cells. There is a 5-15% chance of metastasis to lymph nodes. This prostate cancer may have rapid invasive growth. Treatment includes prostate removal (prostatectomy) + radiotherapy. |
| 8 (4 + 4) | 4 | 63,6% | Aggressive low-differentiated adenocarcinoma. Treatment includes radiotherapy or radical prostatectomy followed by antiandrogens. |
| 9 – 10 (4 + 5, 5 + 4, 5 +5) | 5 | 48,9% | Highly malignant adenocarcinoma. It is characterized by rapid growth and high rate of distant metastases. Therapy includes prostatectomy, radiation therapy, hormone therapy + metastasis treatment. |
How much the Gleason score can be trusted. There have been repeated studies where this score was calculated on the basis of histology, the material for which was taken during biopsy and then after removal of the prostate gland. For prostate cancer with a score of 7, the concordance of the results was 85.7%, and with scores of 8-10 - 68% (more often there was an overestimation of the aggressiveness of the neoplasm).
More about TNM
How to read it. The system adopts the following numerical designations:
- T - T0 (no tumor), T1-4 (primary focus is detected and has certain sizes), Tx (insufficient data to determine the primary tumor).
- N (metastases to regional lymph nodes) - N0 (absent), N1 (present), Nx (no data).
- M (distant metastases) - M0 (none), M1 (present), Mx (insufficient data).
For prostate cancer, the regional lymph nodes are those located in the:
- pelvis,
- below the division (bifurcation) of the aorta into the left and right iliac arteries.
These lymph nodes can be affected on the left, right or both sides. If metastases are present in lymph nodes of other groups, for example in the thoracic organ area, they are considered distant and are labelled M1a. M1b means that the cancer cells have travelled to the bones and M1c to other organs.
Stage 1 prostate cancer
Characteristics:
- T1aN0M0,
- ISUP (G) - 1,
- Gleason score - up to 6.
A T1 tumor does not bother the patient (the disease is asymptomatic), the usual medical examination by an andrologist or urologist does not reveal pathological changes either, as the tumor is too small to be palpated with fingers through the rectum (rectal examination).
In this regard, a distinction is made between:
- T1a - incidental detection of a neoplasm during transrectal ultrasound of the prostate, when the number of cancer cells in the histological specimen does not exceed 5%.
- T1b - the same, but the number of cancer cells is more than 5%.
- T1c - the tumor is detected in a fine needls biopsy of the prostate, made after first detecting an elevated level of prostate-specific antigen (PSA).
Stage 1 is diagnosed exclusively in case of T1a. It is characterized by the absence of regional lymph node involvement and distant metastases. With timely treatment, the prognosis is favorable.
Stage 2 prostate cancer
Characteristics:
- T1bc, 2abcN0M0,
- ISUP (G) 2-3 or any group,
- Gleason index - 7 or other value,
- pT- 2.
T2 - the tumor does not extend beyond the prostate gland. It corresponds to the pT2 stage of the pathomorphological classification, when the prostate capsule cancer cells have not yet sprouted.
In this case, the following sub-variants of the disease are distinguished, with the lesion affecting:
- one lobe - T2a (up to its 50%), T2b (>50%);
- two lobes - T2c.
Stage 2 of the disease can either go unnoticed by the patient, or, as the tumor grows, cause impaired urination. And only in some atypical cases, the onset of the disease may be characterized by some other manifestations.
Stage 3 prostate cancer
Characteristics:
- T3N0M0,
- ISUP (G) - 2-3 or any group,
- Gleason score - any, usually at least 7-8.
- pT- 3 (a, b).
The prostate carcinoma in this case has spread through the prostate capsule:
- T3a (pT3a) – the lesion spreading into the surrounding tissue, including the bladder neck, on one or both sides.
- T3b (pT3b) - the seminal vesicles are affected by cancer cells.
At this stage, the disease signs are more varied. Blood in the urine occurs when cancerous cells grow through the urethra or bladder. If the cancerous focus is large enough and has "captured" the neck of the latter, it may compress the ureteral openings, leading, in turn, to urinary retention in the upper parts of the urinary system and even hydronephrosis, when an excessive amount of urine accumulates in the renal collecting system, "stretching" the kidney and, partially or completely, "turning off" its work. Another common complaint is progressive urinary incontinence.
If the tumor has gone beyond the prostate capsule and damaged nearby nerve tissues, erectile dysfunction is possible.
Stage 4 prostate cancer
Characteristics:
- T4N0-1M1,
- ISUP (G) - any grade, usually high.
- Gleason score - any, often at least 8.
- pT- 4.
T4 (pT4) - the primary tumor has overgrown far beyond the prostate gland, spreading into the rectum, muscles of the anterior abdominal wall, pelvic floor, sphincter, etc. In this case, stage 4 can be diagnosed even if there are no distant metastases. On the other hand, it is also established when the primary tumor has not yet gone beyond the prostate, but has already given dropouts to distant lymph nodes and other organs. Based on this, oncologists distinguish the following variants of stage 4 prostate cancer:
| T | N | M | ISUP (G) |
| T4 | 0 | 0 | Any |
| Any T | 1 | 0 | Any |
| Any T | Any N | 1 | Any |
As can be seen from the table, even stage 4 of the disease is not a verdict, but just one of the variants of its course. Today, thanks to the potential of modern medicine, it is possible to achieve a lot even at this stage of the disease. For example, by removing a relatively small maternal tumor and a single distant metastasis. And even with the most unfavorable prognosis there are chances to significantly increase life expectancy and improve its quality.
Symptoms at this stage become pronounced and progressive with the spread of tumor cells in the body and the growth of the primary focus. When the rectum is affected or compressed, the consequences may include:
- impaired defecation,
- pain in the rectum, perineum,
- blood in the faeces.
Damage to the pelvic floor muscles is usually accompanied by pain in the area of the perineum, a feeling of discomfort when sitting. Massive metastasis to the lymph nodes leads to swelling of the lower extremities, external genitalia. There may also be pathological fractures, neurological disorders, etc., depending on the location of specific metastases.
Along with this the so-called paraneoplastic syndrome may be observed, which is also found in other types of malignancies. It includes weight loss, general malaise, weakness, anaemia, exhaustion. Fever usually occurs in case of an infection or decay of some parts of the tumor.
Complications of prostate cancer
In the later stages of the disease, those are mostly related to both the growth of the tumor itself and the spread of metastases. Those that can cause premature death include:
- massive haemorrhage (internal, external) associated with the destruction of a major vessel by the tumor,
- intestinal obstruction if the rectum is affected,
- renal or hepatic failure in decompensation.
Very serious complications affecting the patient quality of life are urinary retention with the subsequent development of hydronephrosis, pathological bone fractures and neurological disorders, which are associated with the spread of metastases to these organs.
Also, in the terminal stage of prostate carcinoma, multi-organ failure can develop. Pain syndrome of varying degrees of severity in the pelvis, lumbar region, perineum occurs when the corresponding nerves are affected.
Metastases
Metastases are new tumor foci that result from the movement of cancer cells from the primary tumor outside the prostate gland. As a rule, the first of them appear when the carcinoma grows through the gland capsule.
In the body, they can spread:
- through blood vessels (haematogenous),
- through the lymphatic system (lymphatic),
- through the serosa to adjacent organs (transcoelomic).
In the case of lymphatic or haematogenous metastasis, several stages are distinguished:
- Intravasation - cancer cells directly entering the lumen of the vessel.
- Dissemination - cancer cells "travelling" in the body with the blood or lymph flow.
- Embolism - "stucking" in a small vessel (capillaries, etc.).
- Extravasation - exit of cancer cells into the peri-vascular tissue.
- The formation and growth of a daughter tumor.
The further fate of these still microscopic neoplasms depends on many factors that scientists have not completely clarified. However, as a result, some of them may fall into a state of "hibernation" and "lie in wait” in this state for several years, or even decades, while others may immediately begin to actively develop. Due to the presence of such microscopic metastases, recurrences of the disease are possible, so even after comprehensive cancer treatment, several years of follow-up monitoring are required.
Regularities. The lower the differentiation of malignant cells, the higher the Gleason score, the higher the likelihood of rapid prostate cancer growth and metastasis.
Risk assessment of lymph node involvement in patients with prostate cancer:
| Stage | Gleason score | Probability of metastasis to lymph nodes | 10-year recurrence-free survival rate |
| T1 – T2a | 2-6 | < 5% | 70-90% |
|
T2b – T2c |
7 | 5-15% | 60-75% |
| T3a | 8-10 | 16-49% | 43-60% |
The organs where metastases occur most often are:
- Bones - often affecting the spine, pelvis, ribs, less frequently the extremities. Cancerous foci cause pain that is poorly controlled by common painkillers, as well as long-healing fractures, deformities.
- Liver - small metastases develop asymptomatically for a long time. As they grow, there is weakness, a feeling of heaviness or dull pain in the right side or in the stomach area. In the case of massive lesions gradually develop varying degrees of liver failure.
- Lungs - as in the case of the liver, metastases in these organs do not make themselves known for a long time. At later stages, there may be a feeling of "heaviness" in the chest, the appearance of dyspnoea, chronic cough.
- Central nervous system - headaches, which may be accompanied by nausea, dizziness; due to compression of the spinal cord a variety of neurological symptoms develop, including paralysis of the limbs and disruption of the pelvic organs.
Diagnosis
Since in the early stages there are practically no warning signals of the disease that the patient can notice, laboratory and imaging tests come to the fore. In men, starting from the age of 45-50 years, they constitute regular preventive examinations, including:
- TRUS (transrectal ultrasound) of the prostate gland
- determination of PSA level.
Complaints. Characteristic of the third or fourth stage of prostate cancer when the tumor goes beyond the prostatic capsule and begins to sprout into the surrounding organs and tissue. However, due to the fact that many carcinomas grow quite slowly, it always makes sense to see a doctor, even if it seems that the process has already gone too far. Because even in such situations, modern medicine allows 3-6 out of 10 patients to live another 5 years or more.
Digital rectal exam (DRE). At the first stages is also a rather uninformative procedure, as it can detect a tumor of at least 0.2 ml in volume. In the case of asymptomatic course of the prostate cancer it allows to suspect oncology only in 0.1-4% of patients. However, at later stages, the diagnostic value of this type of examination increases.
Laboratory tests. First of all, it is the determination of the level of prostate-specific antigen (PSA) in the blood. This analysis is done both for preventive purposes and when the disease is detected to assess the effectiveness of treatment and, in some cases, to decide whether it is necessary to perform a primary or repeat biopsy.
PSA is a protein that is synthesized by prostatic cells. Its level is increased not only in prostate cancer, but also in a number of other diseases, including chronic prostatitis, benign adenoma. In addition, this value can depend on age and taking certain drugs.
| PSA level, ng/ml | Probability of carcinoma, % |
| 0,0-0,5 | 6,6 |
| 0,6-1,0 | 10,1 |
| 1,1-2,0 | 17,0 |
| 2,1-3,0 | 23,9 |
| 3,1-4,0 | 26,9 |
Mean values of normal PSA values depending on age:
| Age | PSA level, ng/ml (average value) | PSA level, ng/ml (normal) |
| 40-49 | 0,7 | 0-2,5 |
| 50-59 | 0,9 | 0-3,5 |
| 60-70 | 1,4 | до 4,5-6,5 |
In international medical practice, it is customary to distinguish the so-called discriminatory PSA level, i.e. the value that requires a more detailed examination. Most oncologists consider this value to be 2.5 ng/ml, although it should be regarded with consideration of age and other factors that may increase or decrease it.
Sometimes, in addition to PSA, an in-depth study of this indicator (modifications) is needed, including:
- Determination of the prostate gland density and transition zones, both values being calculated from TRUSI data as the ratio of the prostate-specific antigen level to the corresponding volume, expressed in cc. cm. Characteristic of prostate cancer are the values >0.15 and >0.35.
- PSA fractions: total PSA, free PSA and the ratio of free to total PSA (in cancer this ratio is <0.1).
- PSA increase rate: an increase above 0.35 ng/ml per year indicates malignancy.
Another test sometimes used for diagnostic purposes is PCA3. It is a substance that is detected in the urine after rectal massage of the gland. Its level increases as the size of the tumor increases. Like other diagnostic tests, it does not offer 100 percent certainty and is not a substitute for other early detection methods, but always just an additional diagnostic component
Prostate Health Index (PHI). This is a complex index based on a formula that combines 3 indicators at once: total, free PSA and its isoform (-2proPSA). PHI avoids up to 20% of unnecessary biopsies.
This index is needed when deciding whether a biopsy is advisable when palpation does not reveal any abnormal features, but the PSA is 2-10 ng/ml.
Other tests. They can be recommended depending on the specific situation and include general clinical studies (general blood count, urine analysis), biochemical indicators that allow to reveal the presence/absence of renal, hepatic insufficiency, etc., and other exams.
Imaging studies
TRUS. This stands for a transrectal ultrasound examination. For its successful performance, the night before, a cleansing enema is administered, and in the morning, if necessary, the intestines are emptied. Before the study it is necessary to empty the bladder. The examination is carried out using a transducer placed in the rectum.
TRUS indications:
- Suspicion of prostate cancer or other disorders,
- Need to improve the accuracy of transrectal biopsy.
Multiparametric MRI (mpMRI) is used when the tumor is located in the anterior prostate and it is not possible to perform a classical biopsy. The method has been shown to be accurate enough to detect tumors with a Gleason score of 7 or higher.
Pathology examination
Biopsy. In the case of prostate cancer, it is performed using two techniques – conventional and fusion.
The conventional biopsy is done by a puncture through the wall of the rectum (transrectally). For this purpose, a device is used that allows taking material from several sites at once. According to modern standards, samples should be taken from at least 8 sites, but preferably from 10-12. The procedure itself is often performed under the ultrasound guidance (TRUS), outpatient and under local anaesthesia. After a conventional biopsy, a course of antibiotic therapy is usually prescribed.
Fusion biopsy is performed under both ultrasound and mpMRI guidance. As a result of overlaying the images, the doctor receives a three-dimensional picture of the organ. This increases the accuracy of the subsequent histological examination, as it allows to avoid “blind” sampling from suspicious areas. As a rule, in this case, samples are obtained from a much larger number of sites, the number of which can be up to 32.
Fusion biopsy is performed under general anaesthesia, often in hospital. The puncture is performed not through the rectum, but through the perineal tissues, so the risk of infection is reduced. In addition, this procedure allows you to "get to" all the hard-to-reach areas, which is impossible to do in the case of a conventional biopsy.
Immunohistochemical examination. The tissue obtained by a biopsy or surgery is usually paraffin-embedded and then cut into very thin plates to allow detailed examination of the sections under a microscope. The accuracy of the subsequent examination depends on how this preparatory stage is carried out.
Slide examination is carried out both by automatic systems and with the participation of highly qualified pathologists. As a result, the tumor type is determined, the Gleason index is calculated, the ISUP prognostic group is calculated, and other features of the neoplasm that are important in each particular case are determined.
If results are equivocal or if there is doubt about the quality of assessment, pathology review may be required.
Metastases and recurrence detection
PSMA PET CT SCAN. This is One of the newest diagnostic techniques that is used to detect recurrence of prostate cancer.
PSMA is a prostate-specific membrane antigen coupled to a radioactive substance (gallium 68). It is injected into the body intravenously and then spreads with the bloodstream throughout the body, "clinging" only to cells initially found only in the prostate gland (the same applies to daughter neoplasms). Normally, all of this antigen should "settle" in the organ itself, but if there is an accumulation in other parts of the body, it indicates metastasis.
One hour after PSMA injection, a computed tomography (CT) scan combined with positron emission tomography (PET) is performed.
Compared to conventional PET with choline, PSMA PET CT allows cancerous foci to be seen, even very small ones. The procedure is indicated if there is a rise in PSA, including doubling (the shorter the time it took, the greater the chance of biochemical recurrence). It can be performed even if the PSA is only 0.2 ng/ml.
| PSA values, ng/ml | Chance of detecting a relapse, % |
| 0,2-1 | 58 |
| 1-2 | 76 |
| >2 | 95 |
Other methods of distant metastases diagnosis.
Those may include:
- PET-CT,
- MRI, CT,
- ultrasound of the abdominal cavity, small pelvis, retroperitoneal space.
Bonde scan and blood alkaline phosphatase activity test are used to detect bone metastases.
Treatment
Since prostate cancer is a group of neoplasms with various malignancy grades, the treatment approach depends on the specific features of the tumor, as well as the age and general health state of the patient.
The available options are:
- active surveillance;
- surgery (e.g. radical prostatectomy, pelvic lymphadenectomy);
- radiotherapy (external, internal, combined);
- drug treatment (antitumor hormones, cytostatics, targeted drugs).
Prognosis. Prevention
A preliminary risk assessment is done using the Gleason score and the ISUP. However, a more accurate idea of the possibility of disease recurrence can be obtained using other evaluation tables and scales. Among them, the most commonly used are the D'Amico classification system and Alan Partin nomograms.
D’Amico classification for prognostic risk factors
This system was proposed in 1998 by Dr. D'Amico, a professor at the Harvard Medical School Radiation Oncology Department. Its purpose is to assess the risk of recurrence after treatment of local cancer. The classification takes into account several factors, including:
- TNM tumor stage (the T index is taken into account).
- PSA level,
- Gleason score.
According to DAmico, there are the following risk groups:
- low - PSA ≤10, Gleason score ≤6, T1-2a;
- medium - PSA 10-20, Gleason score 7, T2b;
- high - PSA >20, Gleason score ≥8, T2c-3a.
Based on these data, tables were compiled to allow a preliminary assessment of the available probability of recurrence in each case, which is important when making treatment decisions. However, in patients with multiple risk factors, other methods of assessing the likelihood of recurrence are required.
Prediction using Partin tables (nomograms)
These tables were developed in 1993 by a group of researchers led by Alan Partin, who at the time was the head of the urology department at Johns Hopkins Medical Centre in Baltimore (USA).
These nomograms are scales based on mathematical models that take into account PSA, TNM tumor stage and Gleason index. The Partin tables include:
- cancer stage from T1c-2c,
- PSA 0-10 ng/ml and greater than 10.0 ng/ml,
- Gleason score - 2-4, 5-6 or 8-10.
How to work with the table. First you need to select the PSA range, then the Gleason index. At the intersection of these parameters are the rows that determine the probability:
- of detecting an organ-restricted tumour,
- extracapsular growth,
- metastasis to lymph nodes,
- seminal vesicle invasion.
These tables were developed for each T1c-2c stage on the basis of multiple studies
Kattan nomogram
The method first appeared in 1999 and still has not lost its importance. At present, specialists use their refined version from 2010. It takes into account the following parameters:
- preoperative PSA level,
- removed tumour Gleason score,
- surgical margin status,
- presence/absence of invasion into the prostate capsule, seminal vesicles, lymph nodes.
Today, doctors use a computer version of the nomogram, which includes an extended prognosis for a particular patient.
Survival prognosis
In the earlier stages of the disease, with timely and adequate treatment, the survival rate is virtually 100%.
At stages 1-2, the survival chances after radical prostatectomy and radiation therapy are:
- relapse-free - 70-90%,
- overall - 85-97%.
If prostate cancer is detected already at the stage of metastatic process, with complex treatment, the average period before the onset of disease progression is 2-3 years.
Prevention
Preventive specific measures affecting the likelihood of developing prostate cancer are not available as of now. Therefore, early detection of the disease is important.

Second opinion
A second opinion from an experienced doctor is a common practice in countries with advanced healthcare. This is especially true for cancer diseases. An experienced specialist:
- Will explain the disease in more detail, answering questions of concern.
- Evaluate an existing examination or treatment plan for compliance with current medical protocols.
- Inform of the latest methods of treating cancer.
Book a consultation on our website to find out the answers to your questions.
Why is it especially important to get a second opinion?
- Often with high PSA values, biopsy does not reveal a malignant tumor. That's why it's important to get an expert opinion. A fusion biopsy may be ordered to clarify the diagnosis.
- Sometimes a wait-and-see tactic is sufficient in this disease. Such a decision in the case of a known malignant nature of the formation must necessarily be confirmed by another expert opinion.
- All possible advantages and disadvantages of surgical treatment must be considered.
- The local specialist may not be aware of innovative treatment options. For example, radionuclide treatment for hormone-resistant cancer, or focal therapy for a low aggressive tumor.
- There is no single treatment strategy for malignant neoplasms, it is selected individually in each case. Therefore, an reliable opinion will not be superfluous in the selection of the most effective treatment.
References
- Zamboglou C, Adebahr S, Huber М / PSMA-PET/MRI-Based Focal Dose Escalation in Patients with Primary Prostate Cancer Treated with Stereotactic Body Radiation Therapy (HypoFocal-SBRT): Study Protocol of a Randomized, Multicentric Phase III Trial//Dtsch Arztebl Int2021 Nov; 13(22): 5795.
- Clara Breidenbach, Lena Ansmann, Nora Tabea Sibert…/ Predictors for the utilization of social service counseling by prostate cancer patients// Dtsch Arztebl Support Care Cancer. 2022; 30(3): 2327–2339; PMCID: PMC8568309, PMID: 34738162.
- Клинические рекомендации Рак предстательной железы МЗО РФ 2020 г. пересмотра (эл. версия) https://sudact.ru/law/klinicheskie-rekomendatsii-rak-predstatelnoi-zhelezy-utv-minzdravom/klinicheskie-rekomendatsii/2/2.4/
- Stamey TA, Yemoto CM, McNeal JE, Sigal BM, Johnstone IM. /Prostate cancer is highly predictable: a prognostic equation based on all morphological variables in radical prostatectomy specimens// J Urol. 2000;163(4):1155-1160. PMID:10737486
- Moch H, Humphrey PA, Ulbright TM, Reuter VE, eds. /WHO Classification of Tumours of the Urinary System and Male Genital Organs// vol. 8. 4th ed. WHO Press; 2016. ISBN-13 (Print Book) 978-92-832-2437-2.


Comments — 3
Иван Менчиков (Астана)
Какая операция дает больше шансов на полное выздоровление, обычная, или с помощью хирургического робота Да Винчи? Где ни проконсультируюсь, у всех врачей свое мнение на этот счет, а хочется получить объективную оценку шансов. У меня обнаружен рак простаты, но пока без местастазов.
Максим
Мне 54 года, раз в год всегда ходил к урологу, все было нормально, никаких проблем. При последнем обследовании выяснилось, что ПСА сильно повышен и на УЗИ видно, что рак простаты. Я в шоке, не знаю, что делать. Врач предлагает операцию. Это же приговор для мужика…
Marina Virko
Принципиально радикальная операция ведет к полному выздоровлению 7 пациентов из 10, при этом впоследствии нельзя исключить проблемы с недержанием или эректильную дисфункцию. Однако современная медицина предлагает помимо операции целый спектр возможностей лечения рака простаты: активное или длительное наблюдение, лучевая терапия, брахитерапия, гормональная и антигормональная терапия. То есть операции можно избежать или по крайней мере ее отложить.