Testicular cancer is not common, but insidious: it hits the young and develops fast.
Finding an experienced doctor and care facility is crucial for effective disease management.
German oncologists rely only on specialized knowledge
This advice is directly related to the fact that not all specialists understand the subtleties of treating malignant testicular tumors, as the disease is actually not so widely spread. Statistically, there is only one testicular cancer patient per urologist in Germany. As a consequence, 30 percent of German patients receive therapy that does not comply with the guidelines of the national professional society. This increases the number of patients who do not fully recover, although with the right approach they could have been completely cured. Mistakes also increase the number of preventable deaths. This is why clinics in Germany are carefully selected and certified to provide re-evaluation. They use a common (anonymous) electronic databank, which allows the exchange of opinions and enhances the expertise of each certified specialist by "external" cases.
Cologne University Hospital is a pillar of confidence
One of the centers of excellence in the treatment of testicular tumors is the Urology Department of the University Hospital of Cologne, which is headed by European- and internationally renowned urologist Professor Axel Heidenreich. The Department often cares for severely ill patients in advanced stages of the disease, which failed to receive the correct or timely treatment in other specialized facilities. Wrong strategies lead to major complications that require a comprehensive approach, so physicians with other medical specialties also take part in the management of such cases. Urologists at the University of Cologne are engaged in ensuring the research basis and developing basic recommendations, integrative therapeutic concepts and innovative methods, which become official guidelines for the treatment of testicular cancer on the national level.
Statistics highlight the risk groups
Every man should be aware of the risks and the rules of early detection. In particular, those who had an undescended testicle as a child are 2.5 to 8.8 times more likely to develop this malignant condition. The risk increases 2-6 times if the father or brother had this type of cancer, although the genetic mechanisms are not yet fully understood. In addition, the high-risk group includes patients who had a tumor of one testicle, so they are encouraged to have a biopsy of the healthy counterpart for preventive purposes.
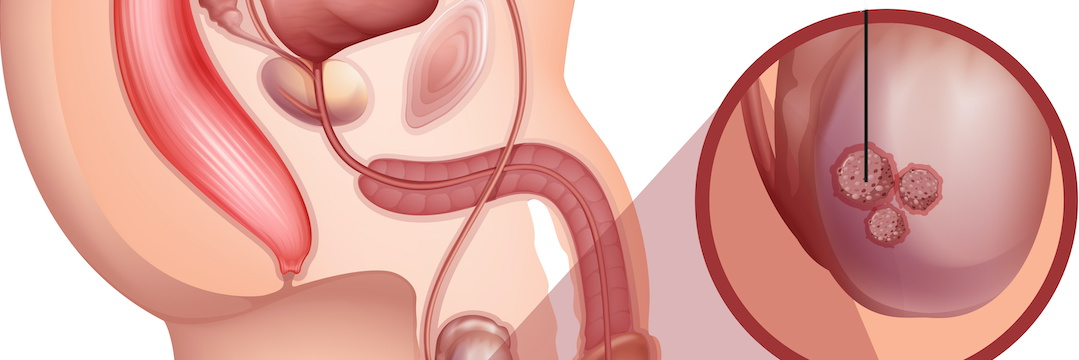
Approximately 90 percent of testicular neoplasms are malignant. They usually develop from so-called pluripotent (capable of forming many of their own kind) stem cells, which under the influence of a number of factors (internal, external, hormonal, genetic) transform into malignant ones. At first, these changes lead to a precancerous state (carcinoma in situ), when the affected cells are not yet able to metastasize. In particular, testicular intraepithelial neoplasia (TIN) is an intermediate stage on the path to degeneration, which, without treatment, inevitably ends in cancer.
Diagnosis must be extremely accurate
A typical sign of testicular cancer is a painless enlargement of the testis, which can be detected by touch. The next diagnostic procedure is sonography and tumor marker blood tests, including alpha-fetoprotein (AFP), chorionic gonadotropin (hCG) and lactate dehydrogenase (LDH).
To reliably confirm or rule out a tumor, inguinal surgical exploration of the testis is performed. If there is no doubt about the presence of a malignant mass, the affected organ is completely removed. For cosmetic purposes, a prosthesis can be implanted in its place.
If in the preoperative stage there is no certainty whether the mass is benign or malignant, testicular enucleation with urgent histology is performed. Experienced pathologists at specialized centers, as a rule, can unmistakably determine the biological nature of the specimens.
In this case, samples are taken from both testicular poles and sent in a special fixing solution for pathology examination and obligatory subsequent immunohistochemical differentiation with strict observance of staining rules. Correct adherence to all requirements ensures error-free detection of testicular interepithelial neoplasia cells.
If malignant lesions of both testicles are confirmed simultaneously or at an interval, a specialized center will offer organ-sparing therapy. The concept developed by Cologne urologists back in 1994 allows them to preserve more than 80 percent of the hormonal activity of patients without long-term risks of relapse. A prerequisite of this approach is mandatory radiation therapy, which destroys the precancerous cells in the partially retained testis.
In this way one can not only achieve the most accurate identification of the tumor, but also detect the presence or absence of its vascular invasion. This information is crucial for planning subsequent therapy. For example, the combination of embryonal carcinoma with affected vessels in the first clinical stage of extragonadal (located outside the testicles) germ cell tumors is very often accompanied by tiny metastases to lymph nodes, which is an indication for adjuvant (preoperative) therapy.
Skillful staging is the key to success
Whenever an extragonadal germ cell tumor is confirmed, advanced diagnostics should be performed to rule out metastases. This is usually done with a CT scan of the chest, abdomen, and pelvis. A PET-CT for primary diagnosis is not necessary.
Evaluation of CT scans, especially those of the retroperitoneal region, must necessarily be performed by a radiologist in collaboration with the treating urologist, with particular attention to the primary lymph drainage pathway from the testicles. This approach enables the detection of interaorto-caval lesions in right-side tumors and pre-aortic and para-aortic masses in left-side conditions, in both cases at the renal vessels level. Adequate evaluation of the lymph nodes requires their measurements in specific projections. A longitudinal diameter of 1 cm in the primary lymph drainage area against the presence of relevant risk factors almost always indicates the presence of micrometastases and requires adequate therapy.
The imaging test results together with the corresponding decrease in the half-life of tumor markers (AFP is 5-7 days; hCG - 24-26 hours) and their absolute values after orchiectomy determine the further prognosis and best therapy choice. The values of tumor markers that do not correspond to a half-decay or plateau are indicative of an unfavorable prognosis and require a change in the therapeutic regimen.
Determination of testicular cancer stages according to the Lugano classification or IGCCCG (International Germ Cell Cancer Consensus Group) is based on the tumor marker values and the spread of the primary lesion. The IGCCCG score is used for progressive metastasis; it determines the intensity of systemic therapy.
Therapy selection needs a comprehensive approach
The Urology Department of the University Hospital in Cologne offers all types of testicular cancer treatment, including:
- surgical removal;
- organ-preserving surgery;
- systemic chemotherapy in the primary stages and at recurrence;
- high-dose chemotherapy with stem cell transplantation;
- Cyberknife for spinal and brain metastases;
- residual tumor resection with metastases after chemotherapy.
Testicular intraepithelial neoplasia treatment
If a testicular biopsy reveals TIN, therapeutic intervention is mandatory.
Only in men with normal spermogram, planning to conceive the wait-and-watch strategy can be used, which will require regular ultrasound monitoring and self-palpation. If a second tumor does manifest itself in such cases, doctors strive to perform organ-preserving enucleation.
A therapy of choice for TIN is local radiation with a total dose of 18-20 Gy. If an intraepithelial tumor is diagnosed as part of fertility testing, surgical removal of the testis is recommended, because local radiation is associated with impaired hormonal function of the healthy testis.
Bilateral germ cell tumor management
In about 3.5 percent of all testicular cancer cases, germ cell tumors develop on both sides, either simultaneously or in succession. Previously, the standard therapy in such cases was removal of both testicles followed by testosterone substitution. Current guidelines give priority to organ-sparing tumor enucleation via inguinal access.
Since then, it has been his routine method; however, he insists that such procedures should only be performed in centers of high competence. Their specialists can take into consideration all aspects which, in aggregate, influence the decision if enucleation is really the best option, such as hormone level and tumor size. Specialized centers also feature better radiation therapy facilities.
According to Cologne University Hospital Urology Department statistics, as well as data provided by peer testicular cancer centers in Germany, patients with preserved organs do not have a higher relapse rate, and their recovery rate is not lower than in those who underwent removal of both testicles. Their hormonal status remains satisfactory, requiring no testosterone substitution.
A second opinion significantly increases success rates
The University of Cologne Urology Clinic does not only provide care to a large number of testicular cancer patients, including the most complicated cases, but also delivers remote advice to those who receive treatment at other healthcare facilities in Germany and around the world. Careful data analysis and expert evaluation of the current treatment compliance with valid clinical guidelines result in recommendations, which very often make considerable changes in the management strategy, ensuring a more favorable prognosis. That is why the department is nationally and internationally recognized as an accredited second opinion center for malignant testicular tumors.
References:
- Albany, C., et al., Multidisciplinary clinic approach improves overall survival outcomes of patients with metastatic germ-cell tumors. Ann Oncol, 2018. 29(2): p. 341-346
- Bertz, J., N. Buttmann-Schweiger, and K. Kraywinkel, Epidemiologie bösartiger Hodentumoren in Deutschland. Der Onkologe, 2017. 23(2): p. 90-96.
- EAU, EAU Guidelines on Testicular Cancer. 2018, European Association of Urology


Comments — 0