
Blood pressure in the blood vessels is an important factor in the work of the cardiovascular system. When it constantly exceeds the norm, the whole body is at risk of irreversible abnormal changes. This condition is called arterial hypertension, which is a serious disease that needs timely treatment.
What is blood pressure?
With each heartbeat, blood (a source of oxygen and nutrients) is pumped into the arteries that carry it to the various organs of the body. As it does so, it presses on the walls of the blood vessels from the inside, creating blood pressure (BP). It determines the blood flow velocity, making sure that the blood gets to where it is needed at the right time. It is measured by two numbers:
- Systolic/Top BP at the moment when the heart muscle contracts (systole) and ejects the blood into the arteries.
- Diastolic/Bottom BP at the moment when the heart muscle relaxes (diastole) and the heart gets filled with blood
The blood pressure is measured in millimeters of mercury (mm Hg).
What affects blood pressure in the blood vessels?
The values depend on factors such as age, gender and lifestyle. Therefore, it is normal for older people to have higher values. There is also a difference between women and men: until the age of 60, men are slightly more likely to suffer from hypertension than women of the same age. Then this ratio changes, as many women have it after menopause.
Time of day also makes a difference. For example, the pressure drops during sleep.
The amount of blood in the body also plays a role: for example, blood loss due to an accident leads to a decrease in arterial pressure. If, for example, a person consumes a lot of salt, which holds water, the increase in blood volume has the opposite effect.
Which values are considered normal and which are indicative of disease?
The ratio of 120/80 is considered optimal. The upper limits of the norm for systolic BP is 130 mm Hg, for diastolic - 85 mm Hg.
Indicators below 100/60 mm Hg indicate hypotension (low blood pressure). It often causes no complaints, but can sometimes manifest with symptoms such as dizziness, headache, fatigue, difficulty concentrating, pallor or fainting. Unless the cause is a medical condition, persistent hypotension is harmless.
On the contrary, with high blood pressure (if the systolic exceeds 140 mmHg, and/or diastolic - 90 mmHg) is associated with risks of serious (primarily cardiovascular), pathologies.
Worldwide, between 1990 and 2021, the number of patients with this problem doubled to about 1.3 billion. At the same time, almost half of patients are unaware of their diagnosis.
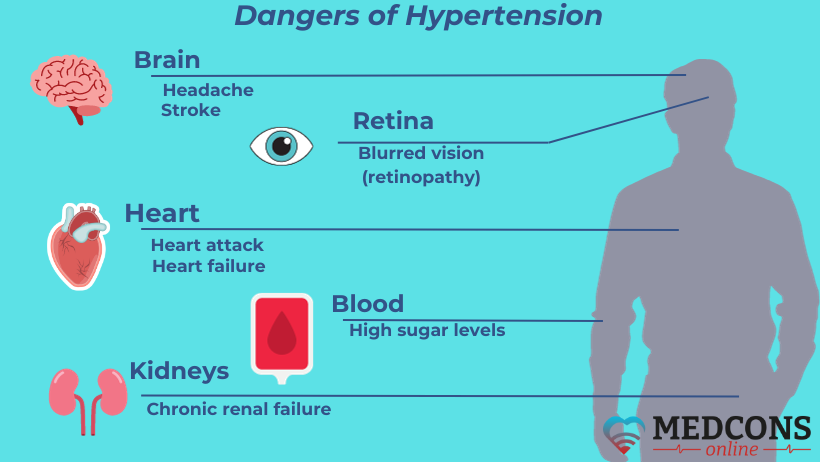
Why is arterial hypertension dangerous?
Constantly elevated pressure does harm to our body, though we do not realize it. First, it damages the arteries. Then, over time, they develop atherosclerosis, get increasingly rigid, start to accumulate fat and calcium deposits, and become narrower. As a result, the arteries can no longer supply the organs with enough blood containing nutrients and oxygen. Pathological changes follow, which, as a rule, are irreversible.
In particular, arterial hypertension can adversely affect the following organs:
The heart: to pump blood throughout the body, it requires more effort, leading to heart failure, an increased risk of heart attack and coronary heart disease.
The brain: hypertension can trigger a stroke or hemorrhage. It also impairs the blood supply to the brain, resulting in the development of vascular dementia.
The kidneys: the damage is chronic kidney disease or even renal failure.
The eyes: abnormal changes occur in the retina, leading to retinopathy.
Lower limb arteries: impaired blood circulation in the legs causes peripheral artery disease.
Symptoms of hypertension
Due to the fact that in most cases the disease does not manifest itself in any way, it is considered particularly dangerous. People suffering from it at first almost do not notice any health decline, so the diagnosis is usually made only at advanced stages, or in connection with secondary conditions. The exception is a severe increase in blood pressure, often called a hypertensive crisis, which can lead to dizziness and visual disturbances.
Arterial hypertension may be indicated by the following signs:
- headache with mental or physical stress;
- morning pain in the back of the head;
- frequent dizziness;
- ringing in the ears;
- nosebleeds;
- shortness of breath during exercise or at rest;
- palpitations;
- recurrent visual disturbances, such as blurred vision;
- sleep disturbances;
- potency disorder (erectile dysfunction).
What are the causes of high blood pressure?
In most people suffering from arterial hypertension, there are no clear causes of the disease. In this case, doctors call it primary or essential. Such a form occurs in about nine out of every ten patients. It is assumed that several factors are involved. For instance, the risk increases with age. Family history may also play a role: if parents or siblings suffer from high blood pressure, the personal risk increases.
Lifestyle also matters. The following factors have an unfavorable influence:
- overweight;
- physical inactivity;
- smoking;
- unhealthy diet;
- excess salt in food;
- permanent stress;
- alcohol abuse.
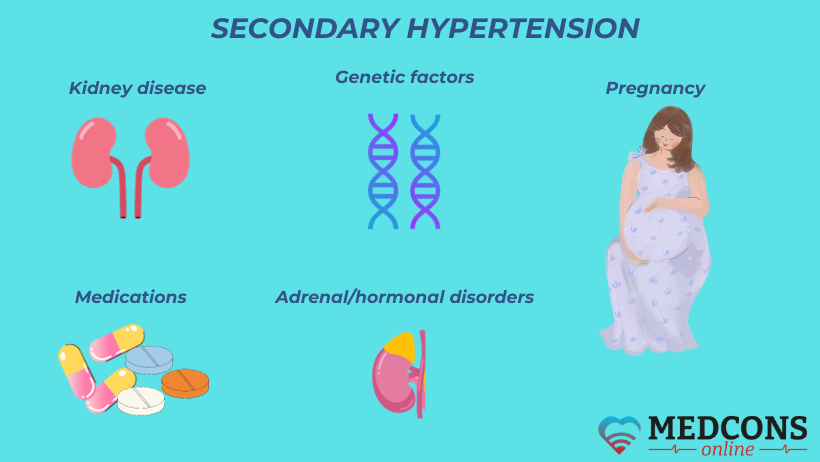
Much less often, arterial hypertension can be associated with a specific cause or condition. In this case, we are talking about secondary hypertension. The secondary type can be provoked by thyroid problems, kidney issues, as well as sleep apnea (stopping to breathe during sleep). Certain medications can also increase the pressure in the blood vessels, such as some painkillers, non-steroidal anti-inflammatory drugs (NSAIDs), nasal decongestants, contraceptives or cortisone.
Classification of hypertension
The current guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH), in addition to the traditional BP classification (optimal, normal, high normal) and hypertension grades, based on the office measurements, recommend categorizing hypertension into three stages depending on the amount of organ damage already present.
Stage I: uncomplicated disease, in which there is no visible damage to organs (including in the presence of chronic renal failure stages 1 and 2).
Stage II: initial abnormalities are present, such as stage 3 renal failure or diabetes mellitus.
Stage III: presence of hypertensive heart disease or advanced chronic kidney disease (stages 4 and 5).
| BP Type/Hypertension Grade | Systolic (mm Hg) | Diastolic (mm Hg) | |
| Optimal | < 120 | and | < 80 |
| Normal | 120-129 | and | 80-84 |
| High-normal | 130-139 | and/or | 85-89 |
| Grade I | 140-159 | and/or | 90-99 |
| Grade II | 160-179 | and/or | 100-109 |
| Grade III | ≥ 180 | and | ≥ 110 |
| Isolated* systolic hypertension | ≥ 140 | and | < 90 |
|
Isolated* diastolic hypertension |
< 140 | and | ≥ 90 |
* In isolated hypertension only one value (systolic or diastolic) is elevated, the other one remaining normal.
How is the diagnosis established?
If hypertension is suspected, the doctor collects an anamnesis, including information about the patient's lifestyle, the presence of such issues as diabetes mellitus, kidney or heart disorders, as well as cardiovascular diseases in close relatives.
Then follows a physical examination, that is, measurement of blood pressure and pulse, determination of body mass index and waist circumference.
An integral component of the diagnosis is a laboratory study of blood (kidney function panel, lipid level) and urine. In most cases, an ECG and ultrasound of the heart and large blood vessels, such as the carotid arteries, are also performed. In some situations, a more thorough examination of the kidneys, brain, or eyes may be necessary.
Hypertension treatment options
As a rule, a combination of therapies is used. Their overall goal is to lower blood pressure and reduce other health risks. All available and necessary treatment options are discussed between the patient and the doctor, and specific target values of BP are meanwhile established.
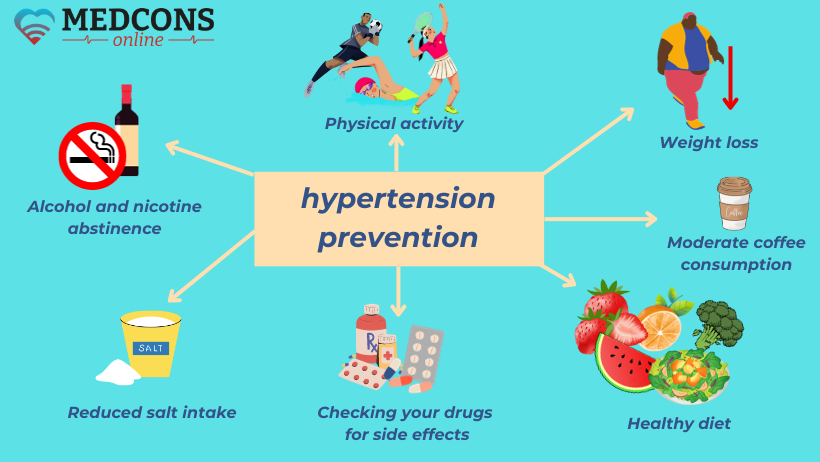
Non-drug therapy and prevention
The very first thing as soon as the diagnoses has been confirmed is lifestyle improvement, which is insisted on by all specialists without exception. It will also help prevent the disease. It is necessary to revise your diet, avoiding too much salt, reducing the amount of carbohydrates and sugar, giving up alcohol.
An equally important therapeutic factor is regular physical activity. It is advisable to have it at least 30 minutes four to five times a week, preferably in the fresh air. For example, walking is ideal for cardiovascular health. Relaxation exercises such as autogenic training, breathing exercises or progressive muscle relaxation are also beneficial.
Blood pressure medications
There are several groups of drugs based on different active ingredients, that are sometimes used in combination. Combining active substances allows them to be used in lower doses, which reduces the risk of side effects.
ACE inhibitors block angiotensin-converting enzyme (ACE) and thereby reduce the hormones that raise blood pressure. For many patients, they are first-line medicines, especially for those with comitant kidney or heart disease. But ACE inhibitors are contraindicated in women who are planning a pregnancy or are already expecting a baby.
Angiotensin receptor blockers (sartans) act similarly to ACE inhibitors.
Calcium channel antagonists inhibit calcium channels in the vascular wall muscles, causing the muscles to relax, which causes the blood vessels to dilate and the pressure to decrease.
Water pills (diuretics) act on the kidneys, increasing urine excretion.
Beta-blockers, in addition to their blood pressure decreasing effect, reduce the heart rate and therefore have a favorable effect on the heart, so they are used in patients with cardiac problems. In asthma, they should be prescribed with caution, as they can worsen the condition.
People react differently to various blood pressure medications, and tolerate them in different ways as well. Sometimes one has to try a number of medications until the optimal type and dosage are found. In this regard, it is worth taking into account the findings of the latest research in the treatment of arterial hypertension: the selection process should be more individualized, and instead of increasing the dose it is advisable to resort to other active substances or groups.
References
- Dieter Schmidt und Christian E Elger. Praktische Epilepsiebehandlung. Praxisorientierte Diagnose und Differentialdiagnose, rationale Therapiestrategien und handlungsorientierte Leitlinien Gebundene Ausgabe – Thieme (1. April 2002)
- G. Wohlrab: Epilepsiebehandlung im Kindes- und Jugendalter: Kontinuität und Wandel. In: Epileptologie, 2003
- Minardi, Carmelo; Minacapelli, Roberta; Valastro, Pietro; Vasile, Francesco; Pitino, Sofia; Pavone, Piero; Astuto, Marinella; Murabito, Paolo (2019). "Epilepsy in Children: From Diagnosis to Treatment with Focus on Emergency". Journal of Clinical Medicine. 8 (1)

Comments — 2
BPCorrect
This is a fantastic and informative post! Understanding blood pressure is so important, and I love how you’ve broken down the details of what’s considered too high or too low in a clear and accessible way. It’s surprising how many people aren’t fully aware of the risks associated with both high and low blood pressure, and the simple explanations really help to drive that message home.
clinical trial translation
Interesting post! Thanks for sharing the information.