Making the heart visible in all its functions and structures in order to detect diseases as early as possible is the main diagnostic task in cardiology. Until relatively recently, the only solution was catheterization, an invasive procedure that involves certain stresses and risks. Today, it can be avoided in many cases with the help of modern radiologic techniques, including cardiac MRI. This exam is practically safe, free of radiation exposure, and provides information significant in quite a number of diagnoses. However, there are some limitations, and certain precautions are necessary.
What and in which way does cardiac magnetic resonance imaging diagnose?
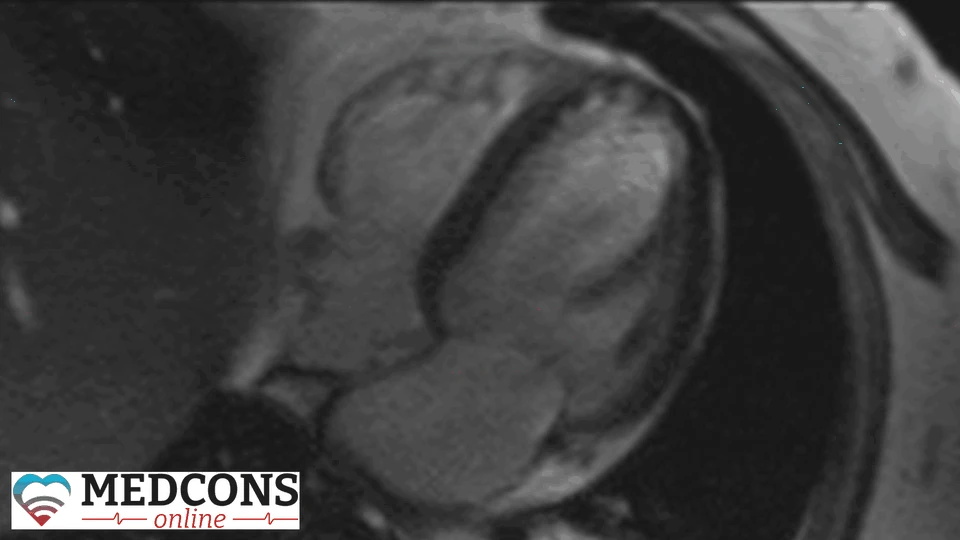
Unlike X-rays and CT scans, MRI uses the properties of magnetic fields and radio waves rather than ionizing radiation. Electromagnetic fields and pulses affect the tiny particles of hydrogen atomic nuclei in the tissues of the human body. The resonance of these particles can be measured, and their signals is convertible into images - transverse and longitudinal slices of the organ under study, in this case - the heart.
The resulting pictures make visible the anatomy of the organ, display the function of the heart chambers and valves, the state of the heart muscle, coronary vessels. In addition, they allow to assess the condition of blood flow.
Indications
The examination can be performed in two different modes – at rest or under stress. There are specific indications for each.
An MRI at rest is used to detect diseases of the heart muscle or heart structures, such as myocarditis or cardiomyopathy. In addition to cardiac function parameters (cardiac output, cardiac volume), the distribution pattern of the injected contrast agent allows for the detection and evaluation of inflammation or scarring.
In the case of congenital and acquired heart defects, it helps to choose treatment strategy, especially if other imaging tests cannot provide clear results.
Magnet resonance imaging can also reveal heart tumors, as well as thrombi in its cavities.
In the case of stressed cardiac magnetic resonance imaging, we are dealing with the so-called pharmacological stress. It is achieved by intravenous administration of a special drug (usually adenosine or regadenoson), which increases the heart rate and dilates the coronary arteries. Simultaneous administration of contrast dye allows to assess the blood flow at an increased heart rate, and to identify areas of heart muscle with reduced perfusion. This type of diagnostics is recommended in the case of suspected circulatory disorders in the heart muscle (myocardial ischaemia).
Cardiac conditions detected by magnetic resonance imaging
With this imaging technique, physicians can diagnose a variety of cardiovascular disorders, including:
- Congenital or acquired abnormalities: valve defects, atrial and ventricular septal defect.
- Circulatory disorders and related conditions: coronary heart disease, heart attack, blood clots.
- Inflammation of the heart muscle or pericardium (myocarditis), cardiomyopathies.
- Storage diseases (genetic syndromes in which abnormal metabolic products accumulate in cells): amyloidosis, haemochromatosis, Fabry disease.
- Vascular disorders.
Are there risk factors?
Decades of clinical practice and the current state of science provide no data proving that magnetic fields as such may have an adverse effect on human health. However, under certain conditions their influence may lead to undesirable consequences. This refers primarily to the presence of any foreign bodies containing metal or special medical devices in the patient's body.
To some extent, a contrast agent can be considered a risk factor as well. Although gadolinium, used in both cardiac scanning and other magnetic resonance imaging studies, is generally well tolerated, it can still cause an allergic reaction in some patients. It can also be a problem for patients with severe kidney disease and pregnant women.
The closed shape of the unit (the narrow tunnel of the magnetic coil) presents a risk of panic attacks, sudden increase in heart and respiratory rate for those who suffer from claustrophobia.
The medication administered for stress MRI poses a health risk for patients with certain severe heart and lung conditions, such as high grade aortic valve stenosis or COPD, and in pregnancy.
Contraindications to MRI of the heart
According to general and specific risk factors, there are cases where the use of magnetic resonance is generally excluded, as well as situations where the technique can be used with certain precautions and limitations.
Absolute contraindications
Patients should not undergo the study if they have:
- Implanted devices (pacemakers, insulin pumps, cochlear implants) except for devices compatible with MRI under certain conditions (MR Conditional).
- Metal particles in critical localization: eyes, brain, chest, etc.
- Extensive tattoos with metal-containing dyes.
Relative contraindications
In the following cases the exam is generally possible, but the risk-benefit ratio must be carefully weighed and, if it is performed, additional precautions must be taken:
| Condition | Commentary |
| Claustrophobia |
Sedatives may be used There are open-bore machines |
| Pregnancy | In some cases, scanning can be performed without contrast or adenosine |
| Contrast agent or adenosine intolerance | |
| Severe renal failure with need for dialysis | MRI is only performed when absolutely necessary |
With some devices the study is not contraindicated as such, but should be done with consideration to certain nuances. These include:
- cardiac electrical activity recorders;
- prosthetic heart valves (except for the earliest models);
- most types of intravascular stents;
- MitraClip (mitral valve repair devices);
- atrial septal defect occluders;
- intrauterine device.
How cardiac MRI is done
The procedure usually lasts between 30 and 45 minutes. A stress MRI may take about 50 to 60 minutes.
Preparing for the study
The doctor explains the procedure and its possible risks, takes the patient’s detailed medical history including allergological anamnesis. Claustrophobic persons may be offered sedation.
Before a conventional cardiac MRI, it is not necessary to abstain from food or water, you can continue to take medication as usual. But if contrast administration is planned, a blood test is done to measure kidney function.
During the examination
No metal objects or devices (jewelry, keys, cell phones, etc.) may be brought into the procedure room.

The patient is placed on a table where an ECG is first performed to monitor heart activity. A surface coil may then be attached to the patient's chest to improve signal quality.
During the procedure, the patient lies inside the MRI scanner; headphones are used to protect against loud noises and to communicate with medical staff.
After the procedure
At the end of the examination, the patient can usually go home without further monitoring. If sedatives have been used because of claustrophobia, you should refrain from driving for a while.
Second Opinion
Magnetic resonance imaging of the heart is not a routine test at most primary care facilities. Even if it is actually required, it may not be suggested if the attending physician is not experienced enough.
While planning heart examinations, especially when invasive procedures (cardiac catheter) are considered, it is advisable to seek a remote cardiology consultation with a more qualified physician to obtain an independent assessment of your case and discuss if magnet resonance imaging might be a good option.
Cardiac MRI should be evaluated by radiologists who have undergone special training and have experience in cardiac imaging. Therefore, to be sure that the interpretation of findings is correct, you can seek an alternative opinion from professionals with the necessary subspecialty.
References
- Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update
- Christopher M. Kramer, Jörg Barkhausen, Chiara Bucciarelli-Ducci, Scott D. Flamm, Raymond J. Kim & Eike Nagel. Journal of Cardiovascular Magnetic Resonance volume 22, Article number: 17 (2020)
- 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Juhani Knuuti, William Wijns, Antti Saraste, Davide Capodanno, Emanuele Barbato, Christian Funck-Brentano, Eva Prescott, Robert F Storey, Christi Deaton, Thomas Cuisset at al. European Heart Journal, Volume 41, Issue 3, 14 January 2020, Pages 407–477
- Durchführung und Befundung der kardialen Magnetresonanztomographie (Kardio-MRT). Positionspapier der Deutschen Gesellschaft für Kardiologie–Herz- und Kreislaufforschung. Kardiologe 2015 · 9:337–347 DOI 10.1007/s12181-015-0021-9 Online publiziert: 9. September 2015

Comments — 0