
Breast masses (or “lumps” in everyday speech) cause anxiety because it might be cancer. However, not all such growths are malignant. For example, fibroadenomas, which often occur in young women, are not cancerous, although they require constant monitoring by a breast care provider.
What is a breast fibroadenoma?
This is a benign tumor resulting from the overgrowth of connective (stromal) and glandular (epithelial) tissue, so it belongs to the group of fibroepithelial neoplasms.
Such masses are felt as dense, mobile nodules with smooth borders, sometimes they can be slightly lumpy. The diameter varies from 5 mm to 5 cm, but usually does not exceed 2-3 cm. Giant fibroadenomas (up to 6 cm) are less common. In five to ten percent of cases, both breasts are affected.
After carcinoma, fibroadenoma is the second most common neoplasm of the female breast and the most common tumor in women under the age of 30. The disease occurs mainly in women and only very rarely in men.
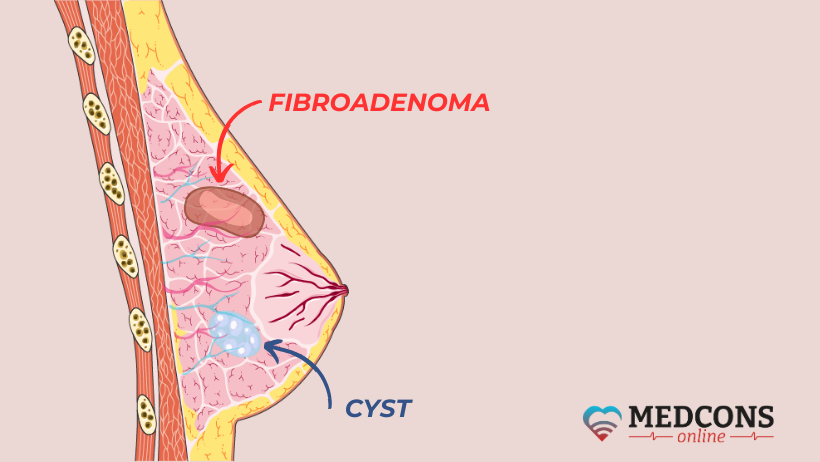
Mastopathy, fibroadenoma, lipoma, cyst: what is the difference?
“Lumps” is a generalized word used in everyday life for any changes in the breast. But in fact, they are fundamentally different.
Mastopathy is more of a collective term for various forms of breast tissue overgrowth. Unlike fibroadenomas, they do not represent true tumors; with the onset of menopause, symptoms no longer appear, and abnormal changes usually disappear.
Lipomas are composed of adipose tissue and are soft to the touch, which is their main distinguishing feature. A cyst is any fluid-filled cavity that is clearly demarcated from the surrounding tissue. The presence of cysts is typical of mastopathy.
Why do fibroadenomas grow?
The exact causes of these breast tumors are unknown, but several factors are thought to contribute to their development.
Reproductive hormone imbalance: abnormal estradiol and progesterone ratio with increased levels of the former. The hormone dependence of fibrous glandular overgrowths is proved, in particular, by the fact that their size partially changes during the menstrual cycle and increases during pregnancy, while regression symptoms (reduction in size, calcification, etc.) often occur in postmenopause.
Familial predisposition: it is known that if fibroadenomas or other benign breast disorders are present in close relatives, the risk of developing these conditions is increased.
Local growth factors: by promoting the proliferation of stromal tissue and glandular components, local growth factors can stimulate the growth of breast lumps.
Injury: it is hypothesized that damage to the organ can induce local tissue changes leading to the development of benign lesions.
Diet and lifestyle: although there is no direct link, some studies suggest that certain dietary and lifestyle factors, such as a high-fat diet, can affect hormone levels and, consequently, stimulate the development of breast nodules.
Other possible causes that are still being debated include certain immunosuppressant drugs and viral infections such as the Eppstein-Barr virus.
Fibroadenoma types
The International Classification of Diseases for Oncology (ICD-O) distinguishes several subtypes of this breast condition, in particular:
- “not otherwise specified” (the most general term, used when the present symptoms are sufficient to make a general diagnosis, but a more specific diagnosis has not been made);
- juvenile;
- intracanalicular;
- pericanalicular.
The difference between the latter two subtypes lies in their growth type. In the intracanalicular variant, the mammary ducts are compressed by a large amount of stromal tissue. In the pericanalicular type, the ducts are wide open and surrounded by stroma.
Juvenile fibradenomas have a specific morphologic structure which includes the pericanalicular growth type with increased stromal cellularity (areas of densely overlapping cell nuclei). The term “juvenile” refers to childhood and adolescence; indeed, these tumors occur mostly before the age of 18, but can form in adults as well. They are characterized by rapid growth and can reach 20 cm in size, requiring surgical removal to restore symmetry.
Symptoms
As a rule, glandular connective tissue masses are asymptomatic. They are often detected accidentally, for example, by palpation or mammography screening. They are mostly painless, but sometimes, especially before menses, may become tender, causing discomfort or mild pain.
Externally, fibroadenomas are inconspicuous except for the juvenile form, which can change the shape and size of the breast due to its large volume.
There are a number of typical signs that indicate the benign nature of a breast lump, namely:
1. It resembles a rubber ball to the touch.
2. It is movable.
3. It has smooth, well-defined edges.
4. It causes only moderate pain and discomfort, mainly during menses.
Diagnosis
If palpation reveals a breast lump, to clarify its nature certain imaging studies are carried consecutively, as well as a biopsy if necessary
On ultrasound breast scans, a typical fibroadenoma has an elongated-oval shape with even borders.
On mammography, these tumors appear as a well-defined foci, sometimes with popcorn-like inclusions (calcifications).
A breast MRI is not a standard procedure for fibroadenomas and is performed, for example, in women who have undergone breast surgery, have silicone implants or have had breast cancer. Also, MRI has a higher sensitivity for dense gland tissue.
Biopsy: although for an experienced cancer care specialist palpation and ultrasound alone are enough to make a relatively accurate guess about the nature of the mass, it is impossible to know what it really is without a tissue sample study.
Histological verification of diagnosis by percutaneous biopsy is appropriate for the following findings:
- equivocal ultrasound findings (BI-RADS 4);
- a tendency to grow confirmed clinically or by ultrasound;
- masses first detected on palpation during menopause;
- solid focal masses in patients with anamnestic risk factors (positive family history, BRCA mutation);
- microcalcifications detected by mammography.
Fibroadenoma treatment
If the diagnosis is confirmed by histolopathology, there is no medical need for removal of such a tumour, especially if its size does not exceed three centimeters and it is not growing. However, even if there is unequivocal proof that there is no malignancy, regular follow-up is necessary. It is usually recommended to self-palpate the breasts monthly and, depending on the recommendations of the attending physician, to perform breast ultrasounds at intervals of three months or more.
Removal of a glandular and connective tissue mass is advisable if:
- it’s large in size (> 3 cm);
- it grows rapidly;
- it causes pain;
- the patient is over 40;
- pregnancy is planned.
Certainly, the procedure can also be performed at the personal request of the patient, if the presence of a mass in the breast brings emotional discomfort and anxiety.
Since the cosmetic outcome is an important aspect of benign breast tumor removal, minimally invasive techniques are increasingly favored.
| Vacuum biopsy | + | Efficiency and cost-effectiveness |
| - |
The likelihood of recurrence and the possibility of incomplete tumor removal Complete excision and maximum cosmetic results can usually be achieved with a tumor size of less than 3 cm |
|
| Cryoablation | + | Absense of pain, efficiency, safety, excellent cosmetic results, no recurrence, positive immunostimulatory side effect |
| - | More suitable for superficial masses | |
| High Intensity Focused Ultrasound (Hifu) | + | Absence of pain, the ability to precisely tailor the exposure to ultrasound beams to the shape of the tumor |
| - | The lack of sufficient efficacy data due to the relative novelty of the technique |
Fibroadenoma vs breast cancer
Like many other benign breast lesions, fibroadenoma is not cancer, that is, it is not characterized by uncontrolled growth and does not metastasize. But whenever any lump is detected, it is necessary to rule out the presence of symptoms that may indicate malignancy, first of all:
- skin changes, such as peeling, redness, an “orange peel” look;
- inverted nipple;
- changes in the shape or size of the breast.
Phyllodes tumor similarities and differences with fibroadenomas Н3
In addition to fibroadenomas, the group of fibroepithelial neoplasms also includes phylloides tumors. They occur much less frequently and are much more difficult to classify and differentiate from histologically similar lesions. The distinction between fibroadenomas and phyllodes tumors is of great clinical significance. The former can be either monitored or removed, and simple enucleation using non-surgical methods is acceptable. In contrast, phyllodes tumors cannot be treated without surgery because they grow rapidly and may be not only benign and borderline, but also malignant. Therefore, extensive surgical excision is necessary with this diagnosis.
What if a fibroadenoma is diagnosed before or during pregnancy?
Hormonal changes during pregnancy can cause breast lumps to grow faster and bring discomfort. For this reason, doctors usually recommend removing even small, asymptomatic and non-growing lesions if conception is planned. The procedure does not affect the ability to breastfeed.
If the tumor is detected while bearing a child, the treatment options are limited due to the risk of harming the fetus. Since it cannot be automatically assumed that the breast lump is benign tissue rather than breast cancer, a breast specialist should be consulted by no means. Tissue sampling can usually be done during pregnancy as well. Further measures depend largely on the results of their histological examination and the individual medical situation.
Menopause
Due to the decrease in the sex hormone levels in women who have already reached menopause, new glandular connective tissue breast growths are very rare. Nodules first detected at this age require special attention and differentiation from malignant diseases.
How can you benefit from a second opinion on fibroadenoma?
Only a few people are able to keep calm when they find some strange lump in their breast. What if it's cancer? Should I believe the scans, or is it better to do a biopsy? Should I rush to a surgeon, or wait, maybe it will go away by itself?
Of course, we encourage you to refer all the questions to a breast care specialist. But seeing only one doctor is not always enough. Here are the most typical situations when a second opinion may be a good idea:
- The radiologist assures me that everything is fine on the ultrasound scan, but I still have doubts, what if this assessment is too optimistic?
- There is nothing wrong by the ultrasound findings, but the mammogram shows suspicious lesions, what should I do?
- A biopsy is scheduled, but is it really necessary to disturb this lump, could it be dangerous?
- The histological report is ambiguous, and the doctor shrugs, saying, let's see if the mass will grow; but what if I miss the right time to act?
- The breast care provider says, I’d better have the lump removed, but if it grows again, will I need another surgery?
There is no need to be ashamed of your doubts and questions, because they are directly related to both physical health and emotional state. An independent assessment by a qualified specialist will help to find a solution in controversial situations, make the right choice, gain confidence and mental balance.
It is important to know that you do not have to visit a doctor personally to get a second opinion on breast fibroadenomas. Remote advice can be no less effective. With the help of modern telecommunication means, you can contact a specialist even in another country, basing your choice on objective data about qualification, practical experience and scientific knowledge. How to do you go about it? We suggest using our second opinion consultation on breast issues.
References
- Stubert, J. et al.: Gutartige Erkrankungen der Brust. Ein Leitfaden für die Praxis. De Gruyter, 2019
- Krings G, Bean GR, Chen YY: Fibroepithelial lesions; The WHO spectrum. Seminars in Diagnostic Pathology, Volume 34, Issue 5, September 2017
- Puay Hoon Tan. Fibroepithelial lesions revisited: implications for diagnosis and management. Modern Pathology Volume 34, Supplement 1, January 2021
- Salati SA. Breast fibroadenomas: a review in the light of current literature. Pol Przegl Chir. 2020.
- Lee M, Soltanian HT. Breast fibroadenomas in adolescents: current perspectives. Adolesc Health Med Ther. 2015

Comments — 0